by Daniel Newman
The Covid-19 pandemic offers fresh proof of the tight relationship between individual health outcomes and the strength of the local economy. New county-level findings from EIG’s Distressed Communities Index (DCI) reveal striking health advantages associated with economic prosperity, showing that economically distressed counties on average have registered nearly two-times as many deaths per capita from Covid-19 as prosperous ones. This graduating relationship between county-level economic well-being and health indicators is present on a range of other outcomes as well.
Since the onset of the pandemic, distressed counties have recorded an average of 529 deaths for every 100,000 residents, whereas in prosperous counties, the rate is nearly half that at 272 deaths per 100,000. To put that difference into perspective: If the average death rate in prosperous places had been as high as that of distressed ones, they would have experienced around 360,000 additional deaths.
Before the pandemic, economically distressed counties exhibited troubling health outcomes that left them more vulnerable to Covid-19
Economically distressed counties were saddled with poor health even before the pandemic struck—burdened by their baseline higher rates of pre-existing health conditions, mortality, and lower life expectancies—all leaving them vulnerable to a virus that attacked such underlying weaknesses. An individual’s level of economic well-being has important implications for the length and quality of someone’s life: Research has shown, for instance, that educational attainment (one of seven factors in a county’s DCI score) is closely linked to mortality rates, and in places where educational attainment runs low, social and economic isolation can bring about worse health conditions and outcomes.
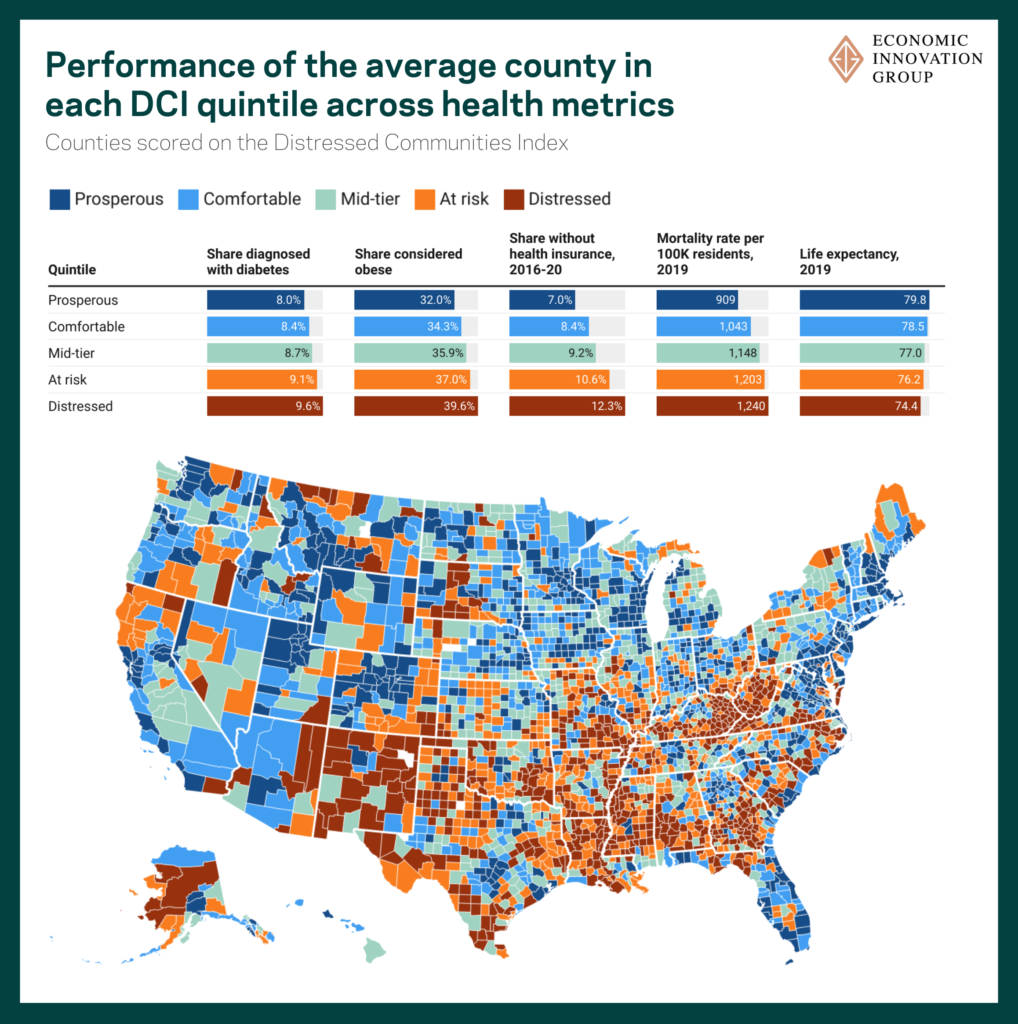
The prevalence of medical conditions considered to be risk factors for Covid-19 complications, such as heart disease and asthma, tend to be elevated in places that exhibit greater economic distress. On two key underlying health risks—diabetes and obesity—less advantaged counties exhibit clearly higher rates relative to more economically advantaged counties. In 2019, the average share of adult residents in a distressed county diagnosed with diabetes stood at 9.6 percent, while in a prosperous county that average was 8.0 percent. The prevalence of obesity among adults was also much higher, with nearly four in 10 considered to be obese in the lowest tier of economic well-being, while that was true for just over three in 10 adults in a prosperous county. Mortality rates, or the number of deaths in a county relative to the size of its population, were on average more than 36 percent higher in distressed counties than their prosperous peers before the pandemic.
These underlying health conditions coexist with a clear disparity in health insurance coverage among tiers of the DCI. The average uninsured rate in distressed counties is 75 percent higher than in the most economically well-off counties across the country. It seems troublingly unsurprising, given the numerous economic and health disadvantages facing many places before the pandemic, that life expectancy for someone born in the average distressed county in 2019 was more than five years lower than for someone born into the top tier of economic well-being.
The gap in vaccination rates between distressed and prosperous counties has failed to close over the course of the pandemic
In addition to underlying health disparities, a lower rate of vaccination against Covid-19 in economically distressed places likely contributed to the stark divergence in deaths between the top and bottom tiers of county-level prosperity. The country’s most economically well-off counties have higher rates of vaccination—which has been highly effective at reducing fatalities and the severity of cases—than any other tier of economic well-being. In the top quintile of counties, 68 percent of all residents were fully vaccinated against Covid-19 through the end of September 2022. The rate steadily declines along the quintiles, reaching a low of 51 percent fully vaccinated in distressed counties.
While early stage distribution of the vaccines faced difficulties in ensuring equitable access across minority and lower income communities, vaccine availability gradually picked up and improved over the course of the vaccine rollout. Nevertheless, there has been a persistent gap between the total share of each quintile’s population that is fully vaccinated, even after vaccines became widely available nationwide. In October 2021, there was a 16 percentage point gap between the share of residents fully vaccinated in prosperous counties (58 percent) and those fully vaccinated in distressed counties (42 percent). Even as the vaccinated population has universally increased over the past year, the gap between the top and bottom tiers of economic well-being has failed to narrow and now stands at 17 percentage points.
Within tiers of economic well-being, metropolitan counties perform better than their more rural counterparts
The urban-rural divide across the United States is one of the country’s clearest differentiators—from voting patterns to earnings and even what kind of restaurants are present—and can be observed in these findings as well. Within each tier of the DCI, metropolitan counties had lower Covid-19 death rates than their non-metropolitan peers. In general, metropolitan counties tend to have better access to health care, are younger, and generally healthier. As the pandemic swept through all corners of the country, the relative advantages present in these more urban locations (perhaps counterintuitively given the infectious nature of the coronavirus and how it is transmitted) has panned out in the health outcomes. At the extreme ends of the spectrum, death rates in distressed, non-metro counties were more than twice as high as in prosperous metro counties.
It seems clear that Covid-19 exacerbated the underlying health disparities present in the United States, resulting in higher death rates and more cases in the most economically distressed counties. While data availability limited this analysis to the county level, the findings likely apply at the zip code scale too, given the tight, place-based linkages between economic and physical well-being across American society. Addressing the economic disparities present across American communities has only gained greater urgency in the light of the pandemic, highlighting how economic conditions have real and consequential effects on health and life, especially as Covid-19 becomes part of a new normal for society. These findings reinforce the importance of a concerted effort to direct resources toward economically distressed places in future health emergencies given the numerous disadvantages they face on this front.





